Acute Pancreatitis
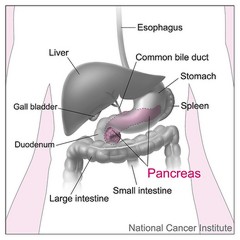
Pancreatitis is
an inflammation in the pancreas. The pancreas is a long, flat gland that lies
behind the stomach in the upper abdomen. The pancreas produces enzymes that
help digestion and hormones that help regulate the way the body processes sugar
(glucose).
In
pancreatitis, the enzymes that are normally released in the digestive tract
begin to affect the pancreas itself. The gland becomes swollen and inflamed.
Numerous enzymes are released into the surrounding tissues and into the
bloodstream.
As a result, digestion
slows down and becomes painful. Other body functions can be affected. The
pancreas can be permanently damaged and scarred if the attacks are severe,
prolonged or frequent.
Symptoms of Acute Pancreatitis
The most common
symptom of acute pancreatitis is pain in the upper part of the abdomen. It can
vary from tolerable to severe.
Pain usually
occurs in the middle of the body, just below the ribs. But sometimes you feel
left or right. This is a constant pain, perforation or "boring". It
can radiate to the back, side, chest or lower abdomen.
- Acute signs and symptoms of pancreatitis include:
- Upper abdominal pain
- Abdominal pain radiating to the back
- Abdominal pain that feels worse after eating
- Temperature
- Fast impulse
- Nausea
- Vomiting
- Tenderness when touching the abdomen
- Chronic signs and symptoms of pancreatitis include:
- Upper abdominal pain
- Lose weight without trying
- Oily and odorous feces (steatorrhea)
Causes of Acute Pancreatitis
Pancreatitis
occurs when digestive enzymes are activated while still in the pancreas,
irritating pancreatic cells and causing inflammation.
With repeated
attacks of acute pancreatitis, pancreatic lesions can occur and lead to chronic
pancreatitis. Scar tissue can form in the pancreas, causing loss of function. A
poorly functioning pancreas can cause digestion and diabetes.
Conditions that
can lead to pancreatitis include:
- Abdominal surgery
- Alcoholism
- Some medicines
- Cystic fibrosis
- Gallstones
- High levels of calcium in the blood (hypercalcemia), which can be caused by an overactive parathyroid gland (hyperparathyroidism)
- High levels of triglycerides in the blood (hypertriglyceridemia)
- Infection
- Abdominal injury
- Obesity
- Pancreatic cancer
- Endoscopic retrograde cholangiopancreatography (ERCP), a procedure used to treat gallstones, can also lead to pancreatitis.
Sometimes, a
cause for pancreatitis is never found.
Risk Factors
Factors that
increase the risk of pancreatitis include:
- Excessive alcohol consumption. Research shows that heavy drinkers (people who drink four to five drinks a day) have an increased risk of pancreatitis.
- Cigarette smoking Smokers are on average three times more likely to develop chronic pancreatitis than nonsmokers. The good news is that quitting smoking reduces the risk by about half
- Obesity. You are more likely to have pancreatitis if you are obese.
- Family history of pancreatitis. The role of genetics is increasingly recognized in chronic pancreatitis. If you are familiar with this condition, your chances increase, especially when combined with other risk factors.
Complications
Pancreatitis
can cause serious complications, including:
- Pseudocyst. Acute pancreatitis can cause fluid and debris to be collected in the cystic pockets of the pancreas. A large broken pseudocyst can cause complications such as internal bleeding and infection.
- The infection. Acute pancreatitis can make the pancreas vulnerable to bacteria and infections. Pancreatic infections are severe and require intensive treatment, such as surgery to remove infected tissue.
- Renal impairment Acute pancreatitis can cause kidney failure, which can be treated with dialysis if kidney failure is severe and persistent.
- Respiratory problems Acute pancreatitis can cause chemical changes in the body that affect lung function, causing blood oxygen levels to drop to dangerous levels.
- Diabetes. Damage to insulin-producing cells in the pancreas caused by chronic pancreatitis can lead to diabetes, a disease that affects the way the body uses blood sugar.
- Malnutrition. Both acute and chronic pancreatitis can cause the pancreas to produce less of the enzymes needed to break down and process nutrients from the foods you eat. This can lead to malnutrition, diarrhea and weight loss, although it is possible to eat the same food or the same amount of food.
- Pancreatic cancer Prolonged inflammation in the pancreas caused by chronic pancreatitis is a risk factor for the development of pancreatic cancer.
Prevention
Avoiding heavy
alcohol consumption will help prevent pancreatitis. Anyone who has ever had an
episode of pancreatitis caused by alcohol should stop drinking completely. This
is essential to prevent a return or become chronic.
Most early
episodes of acute pancreatitis unrelated to alcohol cannot be prevented.
However, taking measures to prevent gallstones can help prevent acute
pancreatitis related to calculus in wounds. To prevent gallstones, maintain a
normal weight and avoid rapid weight loss.
If the cause is
gallstones, gallbladder surgery is usually recommended to prevent future attacks.
When a drug is the probable cause, it will be stopped if possible.
Treatment
If you suspect
you have acute pancreatitis, do not eat or drink until you see a doctor. Eating
and drinking triggers the release of enzymes from the pancreas. This will aggravate
the pain. Most people who develop pancreatitis are hospitalized. They are
treated with painkillers and intravenous fluids.
You will not be
allowed to eat or drink until your symptoms start to improve. In most cases,
nothing can be done to speed up healing or reduce an episode. If the episode is
prolonged and a patient cannot eat more than a week, nutrition can be
administered intravenously.


Hi,
ReplyDeleteTook Onglyza off and on for a year. I have an enlarged adrenal gland. Still I await the outcome of that CT, but I know that much. Will find out more.
I had the CT because of chronic pancreatic pain that started out as "attacks" from a couple of times a month to finally after 3 months of use without interruption, "attacks" 2-3 times a week. My PA put Onglyza on my allergies list.
In the meantime, I lost almost 50 lbs in 5 months due to illness. Loss of appetite, pancreatic pain, chronic diarrhea, then eventually, inability to move my bowels. Severe back pain from the pancreas, and severe chest pain sent me to the ER where I was worked up for cardiac pain. I was cardiac cleared, but told my amylase was very low.
Still seeking a diagnosis, but I lay the blame squarely on Onglyza. I'd had pancreatic issues in the past, and argued with the PA that prescribed it, she was calling me non-compliant, and I feared repercussion from my insurance company.
I even took an article about the dangers of Onglyza, particularly in patients with a history, and she made me feel foolish.
I wish I had listened to my instincts, I fear not only damage to my pancreas that is irreversible, but also severe damage to my left kidney, though I have bilateral kidney pain.
I was off all diabetes meds, and control sugars strictly low to no carb. I can barely eat anymore, I have severe anorexia.
I would warn anyone taking Onglyza to consider a change and try Dr Itua Herbal Medicine, and anyone considering taking it, to select a different avenue. I have been suffering severely for about 9 months, but the past 7 months have been good with the help of Dr Itua herbal medicine which I took for 4 weeks.
I have been off Onglyza now, for 7 months, and simply 100% improvement with the help of Dr Itua. I had none of these issues except a history of pancreatitis in my distant past.
I will recommend anyone here with health problem to contact Dr Itua on drituaherbalcenter@gmail.com and whatsapp +2348149277967 also he ccure the following disease with his herbal medicines Hiv/Aids,Herpes,Copd, Glaucoma, Cataracts,Macular degeneration,Cardiovascular disease,Lung disease, Enlarged prostate, Alzheimer's disease, Dementia. Fibroid,Diabete, Multiple Sclerosis, Hypertension,Fibromyalgia,Hiv, Hepatitis B, Liver/Kidney Inflammatory,parkinson,cancer,als.